What is Signal Intensity in MRI in 2025: A Comprehensive Overview
Author: Jameson Richman Expert
Published On: 2025-08-15
Prepared by Jameson Richman and our team of experts with over a decade of experience in cryptocurrency and digital asset analysis. Learn more about us.
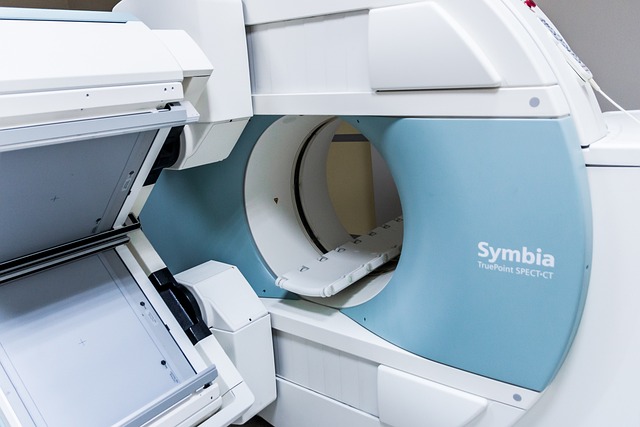
Understanding what signal intensity in MRI is crucial for clinicians, radiologists, and medical researchers aiming for precise image interpretation and optimized patient care. As of 2025, Magnetic Resonance Imaging (MRI) continues to evolve rapidly, integrating advanced physics, quantitative metrics, molecular imaging, and artificial intelligence (AI) to deepen our understanding of tissue characteristics. This comprehensive overview explores the physics behind signal intensity, its clinical significance, technological innovations, and future directions. Mastery of these concepts enhances diagnostic accuracy, supports personalized medicine, and opens new horizons for research and therapeutic strategies.

Defining Signal Intensity in MRI
Signal intensity in MRI refers to the relative brightness or darkness of a specific region within an image, representing the magnitude of RF signals emitted by hydrogen protons in tissues. It is a vital visual indicator of tissue composition, hydration, molecular environment, and pathological changes. Unlike direct tissue measurement, signal intensity is a composite parameter influenced by multiple tissue properties and technical factors. Clinically, analyzing variations in signal intensity assists in differentiating tissue types, identifying abnormalities such as tumors, edema, hemorrhages, and degenerative processes, and monitoring disease progression or response to therapy with high sensitivity and specificity.
The Physics Behind Signal Intensity
Rooted in nuclear magnetic resonance (NMR) physics, signal intensity depends on the behavior of hydrogen nuclei subjected to a strong magnetic field. When placed in a magnetic field (B₀), protons align with the field, creating a net magnetization vector along B₀. Radiofrequency (RF) pulses then tip this magnetization into the transverse plane, producing detectable RF signals as protons relax back to equilibrium. The key relaxation processes governing these signals are:
- T1 relaxation (longitudinal relaxation): The time constant for protons to realign with the external magnetic field after RF excitation. Tissues with short T1 times (e.g., fat) recover rapidly, resulting in high signal in T1-weighted images. Short T1 times facilitate detailed anatomical delineation.
- T2 relaxation (transverse relaxation): The time over which proton spins lose phase coherence in the transverse plane, leading to signal decay. Tissues with long T2 times (e.g., cerebrospinal fluid) produce high signals on T2-weighted images, highlighting fluid-filled spaces and inflammatory changes.
Beyond relaxation, tissue proton density (number of hydrogen nuclei per unit volume) significantly influences signal intensity. The interplay between T1, T2, proton density, and sequence parameters (TE, TR, flip angle, bandwidth) shapes the final image contrast. Advances in 2025 include ultrafast sequences and multi-parametric approaches, which enhance tissue characterization by combining multiple relaxation and diffusion metrics, thereby improving sensitivity and specificity in detecting subtle pathological changes.
Factors Influencing Signal Intensity
1. Tissue Characteristics
Intrinsic tissue properties profoundly affect signal intensity. Fat’s high lipid content yields short T1 and T2 times, producing bright signals in T1-weighted images, helpful for visualizing marrow and subcutaneous fat. Conversely, water-rich tissues like cerebrospinal fluid or edema exhibit long T2 times, appearing hyperintense on T2-weighted images and thus accentuating pathological fluid accumulations, inflammation, or necrosis. Tumor tissues often have altered relaxation times due to high cellularity, necrosis, or edema, which can be exploited for differentiation. Additionally, tissue microstructure, mineralization, and molecular makeup influence relaxation times and susceptibility effects, affecting signal appearance. In 2025, quantitative tissue mapping enables precise measurement of these properties, leading to more accurate tissue classification and disease characterization.
2. MRI Sequence and Technical Parameters
The specific MRI sequence chosen (e.g., T1-weighted, T2-weighted, FLAIR, diffusion-weighted imaging) directly impacts the observed signal intensity. Short TR and TE sequences (like T1-weighted) emphasize differences between fat and water, aiding in anatomical detail. Longer TR and TE (T2-weighted) sequences highlight fluid and edema. Fine-tuning parameters such as TE, TR, flip angle, and bandwidth allows clinicians to optimize contrast for specific tissues or pathologies. For example, increasing TE enhances T2 contrast, aiding in detecting subtle fluid changes. The use of advanced techniques like inversion recovery, fat suppression, susceptibility-weighted imaging (SWI), and chemical shift imaging has been refined to improve lesion conspicuity and tissue differentiation. In 2025, these adjustments are often guided by AI algorithms that optimize sequence parameters for individual patient anatomy and clinical questions.
3. Contrast Agents and Molecular Imaging
Gadolinium-based contrast agents (GBCAs) have historically enhanced MRI's diagnostic utility by shortening T1 relaxation times in targeted tissues, increasing signal intensity in lesions such as tumors, vascular malformations, or regions with disrupted blood-brain barriers. Recent innovations include targeted molecular contrast agents, which bind to specific biomarkers like receptors (e.g., integrins, VEGF receptors) or enzymes, enabling functional and molecular imaging with enhanced specificity. These agents facilitate early detection of pathology at the cellular or molecular level, support theranostic applications, and contribute to personalized treatment planning. Advances in nanoparticle-based contrast agents and biodegradable options further improve safety and effectiveness, making molecular imaging more accessible and informative in 2025.
Clinical Significance of Signal Intensity
Accurate interpretation of signal intensity variations is foundational to MRI diagnostics. Recognizing characteristic and atypical signal patterns allows clinicians to differentiate normal from pathological tissues, assess disease activity, and evaluate treatment response:
- Neurological Imaging: White matter appears hypointense relative to gray matter on T2-weighted images. Demyelinating lesions, such as multiple sclerosis plaques, are hyperintense, indicating active inflammation or degeneration. Quantitative susceptibility mapping (QSM) enhances detection of iron deposits, microbleeds, or calcifications, providing additional diagnostic information.
- Musculoskeletal MRI: Edema, inflammation, hemorrhage, and necrosis display increased signal on T2-weighted images. Novel sequences differentiate between acute and chronic injuries, assisting in precise management decisions.
- Cancer Imaging: Tumors exhibit specific signal patterns; for example, high-grade gliomas often show heterogeneous enhancement, necrosis, and infiltrative margins. Multiparametric MRI—combining diffusion, perfusion, and spectroscopy—provides comprehensive tumor profiles, informing prognosis and therapy planning.
In 2025, quantitative analysis and AI-driven pattern recognition enhance the detection of subtle changes in signal intensity that might precede overt clinical symptoms, facilitating earlier diagnosis and intervention. Continual education on evolving signal patterns and advanced imaging techniques is essential for practitioners.
The Evolution of Signal Intensity Analysis in 2025
Quantitative MRI and Standardization
The transition from purely qualitative to quantitative MRI has been transformative. Techniques like relaxometry, diffusion tensor imaging (DTI), arterial spin labeling (ASL), and magnetic resonance fingerprinting (MRF) now provide absolute measurements of tissue parameters—such as T1, T2, proton density, diffusion coefficients, and perfusion metrics. These metrics serve as objective biomarkers for disease staging, early detection, and therapy monitoring. Standardized protocols across institutions ensure reproducibility and facilitate large-scale multicenter studies, promoting consistency in diagnosis and tracking disease progression over time.
Artificial Intelligence and Machine Learning Integration
AI and machine learning (ML) algorithms have become integral to MRI analysis workflows. Deep learning models trained on extensive datasets can automatically detect, segment, and classify lesions based on complex signal patterns, reducing interobserver variability and accelerating diagnosis. AI enhances sensitivity to subtle pathological changes, such as microvascular alterations, minute tumor nodules, or early ischemic regions, which can be critical in acute settings. Additionally, AI assists in quantitative tissue parameter estimation, predicts disease trajectories, and personalizes treatment strategies, revolutionizing MRI diagnostics in 2025.
Advanced Imaging Techniques and Their Impact
- Diffusion-Weighted Imaging (DWI): Exploits water molecule movement, with restricted diffusion indicating high cellularity—crucial in stroke assessment, tumor grading, and infectious diseases. DTI further characterizes white matter tract integrity and connectivity.
- Perfusion MRI: Measures cerebral blood flow (CBF) and volume (CBV), providing insights into tissue viability, angiogenesis in tumors, and ischemic regions. Techniques like dynamic susceptibility contrast (DSC) and arterial spin labeling (ASL) are refined for higher spatial and temporal resolution.
- Quantitative Susceptibility Mapping (QSM): Maps magnetic susceptibility variations, aiding in detecting microbleeds, mineral deposits, and calcifications with high spatial accuracy.
Future Perspectives and Ethical Considerations
As MRI advances toward higher resolution, multi-parametric, and molecular imaging, ethical considerations become paramount. These include data privacy, equitable access, and transparency of AI algorithms. Developing robust regulatory frameworks, validation standards, and guidelines for integrating quantitative and AI-derived metrics is essential to ensure safe, effective clinical translation. Addressing algorithmic bias, ensuring interpretability, and maintaining patient trust will be critical as these technologies become standard components of diagnostic protocols in 2025 and beyond. Equitable dissemination of innovations globally will be vital to prevent widening healthcare disparities.
Conclusion
Signal intensity remains a cornerstone of MRI, linking fundamental physics with clinical practice. As technological innovations—including quantitative imaging, AI, and molecular contrast agents—continue to develop, our ability to interpret tissue properties with unmatched precision expands in 2025. Deep understanding of the factors influencing signal intensity enhances diagnostic confidence, informs personalized treatment, and accelerates research breakthroughs. For practitioners dedicated to lifelong learning, embracing these advances will unlock new potentialities, ultimately improving patient outcomes and advancing the frontiers of medical science.